Gene therapy is redefining modern medicine with its successes in hematological cancers and recent advances in treating solid tumors, particularly synovial sarcoma.
Gene therapy is on the rise. Having made its first steps at the end of the 20th century, it has since accumulated several successes. This revolutionary approach, which involves modifying the genetic material (and thus the DNA) of cells to cure various pathologies, is now emerging as the cornerstone of what could be called new medicine. Hundreds of clinical trials are currently underway to test the efficacy and safety of this so-called innovative therapy. It aims to treat a range of hereditary diseases (such as severe combined immunodeficiency in “bubble babies,” Duchenne muscular dystrophy—a serious neuromuscular disease—and beta-thalassemia, among others) as well as acquired conditions (including neurodegenerative diseases, heart diseases, ophthalmic disorders and especially cancer) affecting various body systems.
A New Pillar
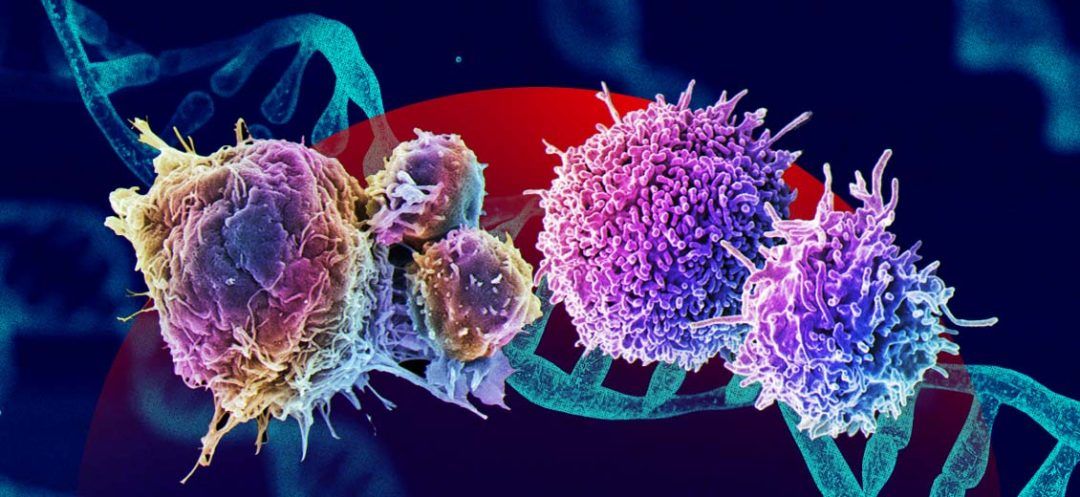
In the realm of cancer treatment, gene therapy has emerged as a vital tool, particularly in hematological cancers. Between August 2017 and February 2022, the FDA approved six treatments based on genetically engineered T cells (a type of immune cell). This therapeutic strategy involves extracting and then modifying, in the laboratory, the patient's own lymphocytes so they can recognize a specific target present on tumor cells. Once reinfused into the patient, these therapeutic cells can specifically target and destroy cancerous cells. This cellular therapy (i.e., a treatment based on cells rather than molecules) now stands as a new pillar of cancer treatment, alongside surgery, chemotherapy, radiation therapy, immunotherapy and targeted therapy.
Challenges and Failures
While gene therapy has led to complete remissions in some hematological cancers, notably acute lymphoblastic leukemias and certain lymphomas, clinical results in so-called solid cancers have been less promising. These tumors are surrounded by a complex tumor microenvironment hindering immune cell penetration and effective tumor destruction. Furthermore, healthy and cancerous cells often share similar markers, complicating the targeting of solid tumors and increasing the risk of toxicity and side effects. Finally, the heterogeneity of tumor cells within solid cancers renders the design of suitable and durable gene therapies challenging.
First Success
On August 2, the FDA announced the accelerated approval of the first gene therapy for adult patients with a solid tumor: non-resectable or metastatic synovial sarcoma (a rare and aggressive soft tissue tumor) in patients who have already been treated with chemotherapy. According to epidemiological data, this cancer affects about 1,000 people annually in the United States, primarily occurring in men in their thirties or younger. Conventional treatment typically involves surgery to remove the tumor, and may also include radiation therapy and/or chemotherapy if the tumor is larger, recurrent or metastatic.
This approval represents a substantial leap forward in the treatment of synovial sarcoma, providing the first new therapeutic option for patients with this cancer in over a decade. It involves a therapy based on genetically modified T cells expressing a receptor against a tumor target (MAGE-A4), expressed by this sarcoma. The FDA’s decision is based on the results of a clinical trial showing an overall response rate of 43.2% and a complete response rate of 4.5%. The median duration of response was six months. It should be noted that the FDA can grant accelerated approval to drugs for serious or life-threatening diseases where there is an unmet medical need. Meanwhile, the pharmaceutical company is conducting further trials to confirm the predicted clinical benefit.
By adopting a targeted and personalized approach, gene therapy ushers in a new era in the fight against the complex and devastating disease known as cancer.
Read more




Comments